GLOSSARY
Amniocentesis
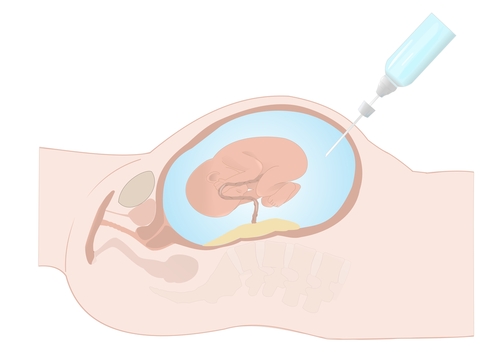
Amniocentesis is a diagnostic test to detect chromosomal abnormalities in the fetus.
Indications for Amniocentesis:
- Women who have screened high risk for chromosomal abnormalities.
- Previous child with chromosomal abnormality.
- Screening for conditions such as Cystic Fibrosis, Thalassemia, or rare metabolic disorders.
- Family history of chromosomal rearrangements
- Fetal abnormality detected on ultrasound
Other Common Chromosomal Abnormalities:
- Trisomy 18 – Edwards syndrome (usually lethal)
- Trisomy 13 – Patau syndrome (usually lethal)
- XO – Turners syndrome (infertile females)
- XXY – Klinefelters syndrome (infertile males)
When is it performed? Amniocentesis is performed after 15 weeks and takes a sample of fluid from around the baby. Amniocentesis is performed by passing the needle through the mother’s abdominal wall. A sterile technique is used to reduce the risk of infection and pregnancy loss.
What will happen on the day of the test? The doctor will explain the procedure in detail, and answer any questions. You will be asked to sign a consent form for the procedure. The procedure is performed under ultrasound guidance.
There is a small amount of discomfort with this test. Most women find that these tests are like a sharp scratch and are well tolerated. The whole procedure takes only a few minutes. After the procedure is completed, the doctor will check the fetal heart rate. All women are asked to wait 15-30 minutes before leaving to ensure women do not feel faint.
We encourage you to have someone drive you home just in case you feel a little pain or faint, however, most women are quite capable of driving themselves home if necessary. We recommend that patients rest at home until the following day and avoid heavy housework or lifting.
If you have a negative blood group, you will require an Anti D injection.
What complications can occur?
- Miscarriage. Amniocentesis has a small risk of miscarriage. If a miscarriage occurs due to an Amniocentesis it usually happens within 2 weeks of the procedure. In experienced hands the risk of miscarriage is very low.
- Bleeding. Is a rare complication. If it occurs, we advise that you contact your doctor immediately or attend the emergency department of your nearest hospital. Most women who have bleeding will go on to have a normal healthy baby.
- Fluid Leakage. This is a rare complication of Amniocentesis and often will stop spontaneously, but in a small proportion it may lead to ongoing loss and miscarriage. If you suspect any fluid loss you should contact your doctor so that it can be confirmed or excluded.
- Transmission of viral infections. There is a very small (theoretical) risk of transmission of HIV, Hepatitis B or Hepatitis C to the fetus if you carry one of these infections. We will ask your doctor to provide us with these test results before we undertake this procedure to ensure that we minimise the risk of this happening to your baby.
- Fetal risk. With Amniocentesis after 15 weeks there are no reported fetal abnormalities due to the tests. Some fetal abnormalities will be discovered at a later date, which are not due to the test, but would have occurred anyway. Because of this, all women are offered a scan at 19 to 20 weeks to try and detect this sort of problem
- Laboratory failure. Very rarely there can be a problem in the laboratory, which means that the specimen fails to give a result or may be difficult to interpret, and it may be necessary to repeat a test.
Results
FISH test: The FISH test (Fluorescent In Situ Hybridisation) is designed to test for Trisomy 21 (Down syndrome) and several other common abnormalities. It usually provides a preliminary result in 24 -48 hours. It is not considered a complete test and in all circumstances, the full result will be available in 10 to 14 days. There is no Medicare rebate for this test.
Microarray test: This test provides a detailed genetic analysis of all the chromosomes. The results usually take about 10-14 days. The results may be completely normal but in some cases, a copy number variant or CNV will be identified. CNVs may confirm the presence of a chromosomal problem but sometimes CNVs will be of unknown or uncertain significance. This means that the finding may or may not be associated with fetal abnormality. Sometimes CNVs may be inherited from one of the parents so additional testing from the parents may be required to understand where the CNV has come from. Our experienced Genetic Counsellors and Fetal Medicine Specialists at Western Imaging for Women will be available to interpret these results and explain any further tests required to you.
It is important to note that when having an amniocentesis at Western Imaging for Women, you will be required to pay for the procedure (Medicare rebates are available for Medicare eligible women). You will also receive an invoice from Victorian Clinical Genetics Services (VCGS) for the actual cost of the genetic testing. The genetic testing costs are also eligible for a Medicare rebate.
Cervical Length Scan
Women who have experienced a previous second trimester miscarriage or a previous early preterm birth (before 32 weeks) may benefit from cervical surveillance. Cervical surveillance involves performing a transvaginal ultrasound to assess the length of the cervix. This is usually done every 2 weeks from 14 weeks to 28 weeks. If the cervix appears short, the specialist will discuss the options for treatment with your referring doctor. In some cases, this might involve Progesterone pessaries or insertion of a stitch into the cervix to keep it closed.
Chorionic Villous Sampling
CVS (Chorion Villus Sampling) is a diagnostic test for chromosomal abnormalities of the fetus. CVS is very accurate in the diagnosis of chromosomal abnormalities.
Indications for CVS:
- Women who have screened high risk for chromosomal abnormalities on either NIPT or first trimester combined screening.
- Previous child with chromosomal abnormality
- Testing for conditions such as Cystic Fibrosis, Thalassemia, or rare metabolic disorders.
- Family history of chromosomal rearrangements.
- Further assessment when an abnormality is diagnosed on ultrasound.
Other Common Chromosomal Abnormalities:
- Trisomy 18 – Edwards syndrome (usually lethal)
- Trisomy 13 – Patau syndrome (usually lethal)
- XO – Turners syndrome (infertile females)
- XXY – Klinefelters syndrome (infertile males)
CVS is performed between 11-14 weeks and takes a sample of tissue (the chorionic villi) from behind the placenta. CVS is performed by passing the needle through the mother’s abdominal wall. A sterile technique is used to reduce the risk of infection and pregnancy loss.
What will happen on the day of the test?
The doctor will explain the procedure in detail, and answer any questions.
You will be asked to sign a consent form for the procedure.
The procedure is performed under ultrasound guidance.
There is a small amount of discomfort. Most women find that these tests are like a sharp scratch and are well tolerated. The whole procedure takes only a few minutes. After the procedure is completed the doctor will check the fetal heart rate.
All women are asked to wait 15 – 30 minutes before leaving to ensure women do not feel faint.
We encourage you to have someone drive you home just in case you feel a little pain or faint, however, most women are quite capable of driving themselves home if necessary. We recommend that patients rest at home until the following day and avoid heavy housework or lifting.
If you have a negative blood group, you will require an Anti D injection
What complications can occur?
- Miscarriage. CVS has a small risk of miscarriage. If a miscarriage occurs due to CVS it usually happens within 2 weeks of the procedure. In experienced hands, the risk of miscarriage is very low.
- Bleeding. Bleeding is a rare complication. If it occurs, we advise that you contact your doctor immediately or attend your nearest hospital emergency department. Most women who have bleeding will go on to have a normal healthy baby
- Transmission of viral infections. There is a very small (theoretical) risk of transmission of HIV, Hepatitis B or Hepatitis C to the fetus if you carry one of these infections. We will ask your doctor to provide us with these test results before we undertake this procedure to ensure that we minimise the risk of this happening to your baby.
- Fetal risk. With CVS between 11 and 14 weeks, there are no reported fetal abnormalities due to the test. Some fetal abnormalities will be discovered at a later date, which is not due to the test, but would have occurred anyway. Because of this, all women are offered a scan at 19 to 20 weeks to try and detect this sort of problem.
- Laboratory failure. Very rarely, there can be a problem in the laboratory, which means that the specimen fails to give a result or may be difficult to interpret, and it may be necessary to repeat a test.
- Confined placental mosaicism. Occasionally abnormal chromosomes are detected in only a small proportion of the cells collected. Sometimes this is because only a subgroup of cells located in the placenta has abnormal chromosomes –a condition called confined placental mosaicism. If confined placental mosaicism is suspected, our specialists may recommend an amniocentesis to confirm that the abnormal cells are restricted to the placenta. If the amniocentesis is normal and
there are no abnormalities detected in the baby, you can be reassured that the baby will be healthy. However, pregnancies complicated by confined placental mosaicism carry a very small risk of developing growth problems in the baby so it is important to undertake serial growth ultrasounds during the third trimester to ensure the baby is growing well.
Results
FISH test: The FISH test (Fluorescent In Situ Hybridisation) is designed to test for Trisomy 21 (Down syndrome) and several other common abnormalities. It usually provides a preliminary result in 24 -48 hours. It is not considered a complete test and in all circumstances, the full result will be available in 10 to 14 days. There is no Medicare rebate available for this test.
Microarray test: This test provides a detailed genetic analysis of all the chromosomes. The results usually take about 10-14 days. The results may be completely normal but in some cases a copy number variant or CNV will be identified. CNV’s may confirm the presence of a chromosomal problem but sometimes CNVs will be of unknown or uncertain significance. This means that the finding may or may not be associated with fetal abnormality. Sometimes CNV’s may be inherited from one of the parents so additional testing from the parents may be required to understand where the CNV has come from. Our experienced Genetic Counsellors and Fetal Medicine Specialists at Western Imaging for Women will be available to interpret these results and explain any further tests required to you.
Early Pregnancy Scan
An early pregnancy scan is usually the first ultrasound you will have in a pregnancy. An ultrasound is performed at this stage of pregnancy to:
- Confirm the expected due date
- Determine whether it is a twin pregnancy
- To visualise the heartbeat
- Exclude a miscarriage
- Exclude an ectopic pregnancy (pregnancy in the Fallopian tube). Prior to 7 weeks, it may be too early to acquire this information so you may need to be rebooked for a follow-up scan if we are unable to obtain all the information required. Sometimes, we may need to perform a transvaginal scan to obtain better views of the uterus and pregnancy.
Endometriosis Scan
Endometriosis is a common gynaecological condition in which endometrial-like tissue forms outside the uterus. The condition often causes painful periods or pain during intercourse.
In severe cases, there may be cysts and deep infiltration of the pelvic organs as well as the bowel. Using transvaginal and transabdominal ultrasound with bowel preparation allows good views of this area to make a more extensive assessment of the pelvis. Determining the extent of endometriosis may influence decisions regarding surgery. In severe cases, more time may be required for the surgery. Sometimes, the gynaecologist may request the presence of a bowel surgeon to provide assistance if we suspect the endometriosis is infiltrating the bowel. The Endometriosis scan requires a transvaginal ultrasound scan. This usually takes about 15-30 minutes.
In order to obtain the best possible views for assessing the pelvis for the presence of endometriosis, a light bowel preparation is recommended. If your doctor recommends an endometriosis scan, our staff will provide you with the details of the bowel preparation when your appointment time is confirmed.
Fetal Echo
Fetal Echo is a special ultrasound examination of the fetal heart which is performed by a Fetal and Paediatric Cardiology specialist. This special ultrasound may be recommended if an abnormality is detected. Women who have had a previous baby with a heart problem or a family member with a heart problem can also benefit from having this scan to ensure there is no heart problem this time.
Women who have particular medical problems such as Diabetes, or have been taking particular medications such as Lithium are at increased risk of having a baby with a heart problem. A fetal echo allows a very detailed assessment of the heart structures to ensure that no abnormalities are present.
First Trimester Morphology Ultrasound

The first trimester ultrasound is performed between 11+ 0-13 + 6 weeks. This is an ideal time to assess the baby to exclude certain major abnormalities. The baby is well formed at this stage so we can examine the baby’s head, face, abdomen, stomach, legs and arms. At Western Imaging for Women, we will also examine the heart, as it is sometimes possible to identify major heart problems at this very early stage, even though the size of the baby’s heart is still very small.
If possible, we try to obtain some 3D / 4D pictures of your baby. This allows you to see your baby and provides a great opportunity for you to bond with your unborn baby.
Measuring the nuchal translucency
The nuchal translucency is the fluid found at the back of your baby’s head and neck, just beneath the skin. The thickness of this fluid can be precisely measured; this is called the nuchal translucency (or NT) measurement. Normally the amount of fluid is small, producing a thin NT measurement.
We know that the amount of fluid can increase in the presence of certain conditions, producing a thicker NT measurement. Conditions associated with an increased NT measurement include some chromosome abnormalities (for example, trisomy 13, 18 and 21) and some structural problems (for example, heart abnormalities). An increased NT measurement does not always mean the baby has a problem but it does increase the risk. The NT measurement can also be used in the calculation for the Combined Screening result for Down syndrome (see First trimester combined Screening for Down Syndrome). For women who prefer to have the NIPT test for Down Syndrome Screening, it is still useful to have the NT scan performed as a way of helping to detect abnormalities in the baby and also helping to detect chromosomal problems which may not be detected by NIPT.
First Trimester Combined Screening Test for Down Syndrome
What is the first trimester combined screening test?
First trimester combined screening is performed between 10 and 14 weeks gestation. This test combines a number of different measures together to provide an estimate of the chance that a pregnancy is affected by a chromosome condition, such as Down syndrome. Additional conditions that can be assessed with the first trimester combined screening include Edwards syndrome (Trisomy 18) and Patau syndrome (Trisomy 13)
The test involves two parts:
- A blood test taken between 9-13 weeks gestation to measure two chemicals called PAPP-A and free Beta hCG.
- An ultrasound scan which measures the nuchal translucency measurement (see image below) at 11+0 -13+6 weeks as well as assessment of the presence of the baby’s nasal bone and assessment of the baby’s anatomy.

This information is entered into a computer algorithm together with your age, weight and gestation to calculate the risk of having a baby with one of the chromosomal problems. The accuracy of detecting Down syndrome is approximately 85% by utilising this screening method. Approximately 5% of women will receive an increased risk result using this screening method. This does not necessarily mean that your baby does have Down Syndrome or one of the other chromosomal problems, but we would recommend further assessment to determine whether your baby really does have one of these problems. If the chance of your baby having Down syndrome is increased, you will be offered an appointment with our Genetic Counsellor to discuss options for further testing including non-invasive prenatal screening (NIPT), Chorionic villous sampling (CVS) or Amniocentesis.
First trimester combined screening can additionally provide information which may also be helpful for the management of a pregnancy, such as risk factors for early onset pre-eclampsia or fetal growth restriction.
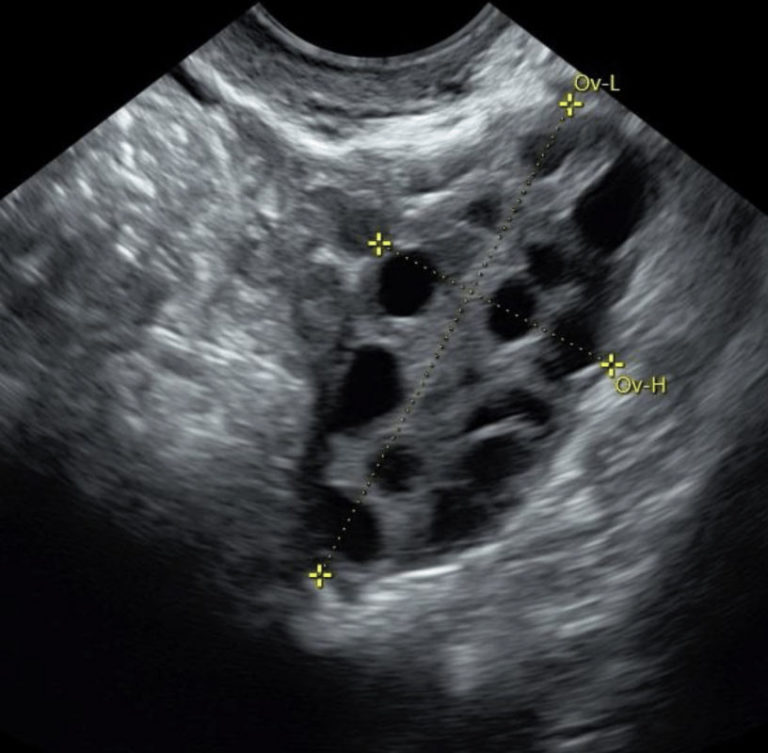
Follicle Tracking
Follicle tracking scans may be required if you are undergoing fertility treatments including IVF or Clomiphene treatment.
Follicle tracking uses transvaginal ultrasound to track the development of egg-containing follicles within the ovary from an immature state to a mature state.
You may be required to have 2-3 follicle tracking scans over the course of your menstrual cycle to assess the number of follicles and rate of growth. The timing of the scans will be determined according to your menstrual cycle and the rate of growth seen in the follicles.
Management of Complex Pregnancy and Fetal Abnormalities
Our specialists have specific expertise in the diagnosis, counselling and management of women with complex pregnancies and fetal anomalies. Appointments can be made with our receptionists by calling 9111 0055. If you have already had an ultrasound scan that shows a fetal abnormality, it is important that you advise us of this when booking your appointment. This will ensure that you are booked to see the appropriate specialist, and also that we allow adequate time to provide any counselling necessary so that we can answer any questions you have and ensure you don’t feel rushed. It is also helpful if you bring copies of your previous ultrasound images so that we can compare images to assess progression as this will help us to determine the likely prognosis.
Placenta praevia: When part of the placenta covers the opening of the cervix (birth canal).
Cephalic presentation: Refers to the head of the fetus being down in the pelvis of the mother.
Breech presentation: Refers to the buttocks, feet or legs of the fetus being down in the pelvis
Aneuploidy: When a fetus has an abnormal number of chromosomes in its cells. The normal fetus has 46 chromosomes in their cells. Aneuploidy may cause a miscarriage or may affect the way the fetus develops. An example of aneuploidy is Down syndrome.
Chromosome: All fetal cells contain strands of DNA called chromosomes. These chromosomes contain the genetic information that determines everything from gender to hair colour.
Renal pelvis dilatation: The renal pelves are spaces within the kidney that collect and help drain urine into tubes (called ureters) that head down to the bladder.
Renal pelvis dilatation is a common finding on ultrasound and may be part of normal development of the fetal kidneys.
Depending on the degree of renal pelvis dilatation, further scans or management may be required. In severe cases, surgery may be required.
Amniocentesis: Amniocentesis is a diagnostic test to detect chromosomal abnormalities in the fetus and is performed after 15 weeks and takes a sample of fluid from around the baby. Amniocentesis is performed by passing the needle through the mother’s abdominal wall. A sterile technique is used to reduce the risk of infection and pregnancy loss.
Infertility: The inability to fall pregnant within 12 months of regular unprotected sex.
Corpus luteum: Is a hormone secreting structure on the ovary which forms after ovulation. The corpus luteum supports the development of the early pregnancy.
Yolk sac: A structure that aids development and growth by providing nutrients to the early pregnancy. It is often the first structure seen within the gestational sac on ultrasound.
Nuchal translucency: The nuchal translucency is the fluid found at the back of your baby’s head and neck, just beneath the skin. The thickness of this fluid can be precisely measured; this is called the nuchal translucency (or NT) measurement.
Nuchal fold: The nuchal fold is a layer of tissue at the back of the baby’s neck that is measured between 18 -22 weeks gestation on ultrasound. A normal measurement is less than 6 mm.
Cerebellum: The cerebellum is a part of the brain that is responsible for movement and balance.
Biometry: Ultrasound measurements used to determine the fetal size and estimated fetal weight (EFW). It consists of four measurements the biparietal diameter, head circumference, abdominal circumference, and femur length.
Cervical length: An ultrasound measurement to assess the length of the cervix. Short cervix lengths are associated with increased risk of preterm labour.
Colour Doppler: Is a non-invasive way of assessing blood flow through blood vessels. Colour Doppler may be used to assess blood flow through structures such as the umbilical cord, heart and brain.
Middle cerebral artery: Is a large branch of the internal carotid artery which supplies the cerebrum of the brain. Colour Doppler interrogation of the middle cerebral artery can be performed to assess fetal hypoxia and fetal anaemia.
Mid Trimester Morphology Ultrasound
Most women will have a scan between 18-22 weeks to assess the fetal anatomy. At this time, the fetus is large enough to be seen clearly and so detailed assessment of many structures can be made, including the below:
- Face
- Brain
- Heart
- Arms and hands
- Legs and feet
- Spine
- Kidneys and bladder
It is not necessary to have a full bladder for this scan; however, some urine in the bladder may make it easier to see structures low in the pelvis.
The friendly staff at Western Imaging for Women will guide you through this ultrasound scan and point out the various features we are looking at. If possible, we try to obtain some 3D / 4D pictures of your baby’s face so you can start to see what your baby is going to look like!
Most of the time, the fetus looks completely healthy and we do not detect any problems. However, occasionally we do identify an abnormality in the fetal growth or development. At Western Imaging for Women, we have a range of Fetal Medicine specialists available to explain the ultrasound findings and what this means for your baby if we do find a fetal abnormality.
NIPT – Non Invasive Prenatal Screening Test with Percept
NIPT (Non Invasive Prenatal screening Test) is a prenatal screening test that uses cell-free fetal DNA found in the maternal blood to identify the most common chromosome conditions found in newborns. The cell-free fetal DNA is released from the placenta into the maternal bloodstream as part of the growth and development of the baby.
This screening is safe and poses no threat to the pregnancy as it uses a simple blood sample collected from the mother. There are many different companies offering NIPT but at Western Imaging for Women we are proud to use the Percept™ test provided by Victorian Clinical Genetics Services (VCGS). The test is performed locally in Melbourne and does not need to be sent interstate or overseas. This means that we can provide you with your results within 3-5 working days.
Percept™can be used to identify pregnancies where there is an increased chance of Down syndrome (trisomy 21), Edwards syndrome (trisomy 18), Patau syndrome (trisomy 13) or sex chromosome conditions such as Turner syndrome (monosomy X) and Klinefelter syndrome (XXY). The chance of having a child with a chromosome condition increases with maternal age. NIPT using Percept™ can also identify rare chromosomal trisomies which may not directly affect your baby but may affect the baby’s growth.
Percept™ can also determine the baby’s gender. This allows you to know whether your baby is male or female well before this is visible on ultrasound.
Percept™ can be used in twin pregnancies as well but it is important to determine whether you are carrying a twin pregnancy on ultrasound before we do this test.
It is important to understand that NIPT with Percept™ has some limitations and cannot detect ALL genetic problems. All patients attending Western Imaging for Women are offered a personalised counselling session with a genetic counsellor or obstetrician with experience in genetics to determine whether this would be the best test for you. We will also discuss whether any additional tests may be recommended.
How do I arrange NIPT through Western Imaging for Women? NIPT with Percept™ can be done any time after 10 weeks’ gestation. A referral from your GP or obstetrician is required for NIPT.
Please call to arrange an appointment (if you do not know your gestation, we can arrange a dating scan prior to your appointment). An ultrasound is performed at your appointment to determine the correct gestation, confirm viability and exclude the presence of major structural abnormalities. You will meet with a Genetic Counsellor or obstetrician to discuss NIPT in more detail and answer any questions you may have.
You will then meet with one of our nurses to have your blood sample collected.
Test Results: Test results are generally available in 3-5 working days and one of our friendly staff members will call you to disclose the result. A genetic counsellor will be available to discuss your results further if you have any questions or concerns.
Receiving a high-risk result does not mean your pregnancy is definitely affected by a particular condition; it means there is an increased chance. In this case, the genetic counsellor will contact you and your referring doctor to discuss further testing options, such as diagnostic testing (using a CVS or amniocentesis). Further testing can be performed at Western Imaging for Women.
If you want the gender disclosed over the telephone we are more than happy to do this. Alternatively, if you would like the gender to be disclosed at a special time of your choosing, we can send you the gender results in the mail. Of course, if you would prefer to keep the gender a secret, you can trust us not to disclose it if you don’t want us to!


Chromosomal Conditions
Down syndrome: Down syndrome is the most common chromosomal cause of intellectual disability. It affects 1 in every 700-900 babies in Victoria. It can occur in any pregnancy regardless of the woman’s age. However, the chance of having a baby with Down syndrome increases with the mother’s age.
Down syndrome refers to an extra chromosome 21. Another name commonly used for Down syndrome is Trisomy 21 (meaning 3 chromosomes of number 21). Babies born with Down syndrome can usually expect to have a healthy long life. The main problem these children face is one of intellectual delay and learning difficulties. Babies with Down syndrome may also have a number of structural abnormalities, such as heart abnormalities.
Down syndrome can be difficult to diagnose with ultrasound alone, hence it is important to consider either NIPT or First Trimester Combined Testing if it is important to you to determine whether the baby could have Down syndrome. Testing for Down syndrome allows people the option to decide whether or not to continue the pregnancy if Down syndrome is detected. The decision about whether to have Down syndrome testing is a very individual one to make.
Further information about Down syndrome can be found at
Edwards’ syndrome: is less common than Down syndrome and is caused by an extra chromosome 18 (trisomy 18). Pregnancies with trisomy 18 often miscarry or result in a stillbirth. Babies that are born alive rarely survive beyond a few weeks of life. All babies with Edwards’ syndrome have significant physical and intellectual problems
Patau syndrome: is even less common than Down syndrome and Edwards syndrome. It is caused by an extra copy of chromosome 13. Pregnancies with trisomy 13 usually miscarry and babies that are live born rarely survive beyond the first few weeks of life. All babies with Patau syndrome have serious health problems.
Sex chromosome conditions: are caused by changes in the number of the X and Y chromosomes present. The X and Y chromosomes determine if a baby will be male or female. Babies with Turner syndrome (monosomy X) are females who have only one X chromosome (X instead of XX). Klinefelter syndrome is not typically associated with miscarriage but can cause some developmental problems and infertility.
Rare autosomal trisomies: NIPT can also detect some additional rare chromosomal abnormalities where there is an additional or third copy of a chromosome. These are known as rare autosomal trisomies. When these conditions are detected by NIPT it can sometimes mean that only the placenta is affected with the trisomy and not the baby. This situation can still sometimes cause serious problems for the normal development of the pregnancy. Knowing this information can help doctors monitor pregnancies at increased risk for complications such as fetal growth restriction.
It is important to understand that NIPT with Percept™ has some limitations and cannot detect ALL genetic problems. All patients attending Western Imaging for Women are offered a personalised counselling session with a genetic counsellor or obstetrician with experience in genetics to determine whether this would be the best test for you. We will also discuss whether any additional tests may be recommended.
Pelvic Scan
For most women, both abdominal and vaginal techniques will be used. However, the transvaginal approach almost always allows clearer views as the ultrasound transducer is closer to the pelvic structures. Prior to the scan, we ask you to empty your bladder for your comfort as well as to optimise views of the pelvic organs.
There are many reasons why your doctor may request a pelvic scan including:
- Bleeding between periods
- Heavy periods
- Period or pelvic pain
- Absence of, or irregular periods
- Excess hair growth
- Possible fibroids
- Suspected pelvic mass
- Difficulty conceiving
- Post-menopausal bleeding
- Screening for ovarian cancer
Timing of scan:
The ultrasound can be performed at any stage of the menstrual cycle to evaluate the cause of pain, however, our preference is to perform the scan shortly after the period has finished. This gives the best visualisation of the lining of the uterus, which should be nice and thin at this time. Just before the period, the lining is thick which makes evaluation more difficult. This might limit our ability to identify the causes of abnormal bleeding due to issues such as polyps. If the lining is too thick, reassessment just after the period may be required.
If polyps are suspected, you will be counselled in detail about the advantages of saline sonohysterography, which might allow better visualisation of the uterine cavity.

Transvaginal Scanning
To perform a vaginal scan, a narrow transducer is placed gently into the vagina and moved close to the cervix, where the views of the uterus and ovaries are best. The transducer is moved gently within the vagina to view all the pelvic organs. This examination may be mildly uncomfortable but is rarely painful. Most women find a vaginal ultrasound more comfortable than a pap smear.
The transducer for transvaginal scanning is covered with a sterile non-latex cover and the transducer is disinfected using approved hospital grade high level disinfection procedures between patients.
Saline Sonohysterography
This procedure is used to diagnose polyps in the lining of the endometrium.
A very thin plastic tube passes through the cervix and into the uterus. This process feels very much like a pap smear test and causes minimal discomfort. The doctor then performs a vaginal scan while inserting a small amount of saline (salt water) into the cavity. The saline outlines any growths within the cavity. This procedure is often performed in addition to a pelvic scan to obtain more information.
It is important to perform this test at the correct time in your cycle to minimise the chance that the procedure itself may unintentionally interrupt a pregnancy. The procedure can be performed between day 2 and day 9 of the menstrual cycle in women who have a regular 28-day menstrual cycle.
In order to book the procedure at the correct time, it is important that you contact us on the first day of your period (or the Monday after your first day if your period starts on the weekend). We will then confirm an appointment date.
Third Trimester Ultrasound

Third trimester ultrasound scans may be required for a number of reasons during your pregnancy including:
- Assessment of the fetal size for babies that are growing bigger or smaller than expected
- Assessment of the location of the placenta
- Review of minor abnormalities in development which were detected early in pregnancy (e.g. review of fetal kidneys when increased fluid is detected in the kidney and pelvis)
During the scan, we will take measurements of the baby which will allow us to calculate an estimate of the baby’s weight. This estimate is not completely accurate but provides a guide to how the baby is growing. It is not necessary to have a full bladder for this scan, but some urine in the bladder may make it easier to see structures low in the pelvis.
In cases where the placenta is low lying and we need to re-examine the location of the placenta, a transvaginal ultrasound may need to be performed. This involves placing a narrow transducer inside the vagina to assess the cervix and measure the distance between the placenta and the cervix. This part of the examination usually only takes 3 or 4 minutes and is completely safe for the pregnancy, even if the placenta is confirmed to still be low lying. You may be asked to go to the bathroom to empty your bladder before this part of the scan. This makes it easier to see the cervix and placental edge as well as making the scan a little more comfortable.
The third trimester is often a good time to obtain 3D or 4D pictures of the baby’s face and provided your baby is in a good position during the scan, we will always do our best to obtain these images for you.
Tubal Patency assessment
This procedure uses a special dye that is used to demonstrate the Fallopian tubes. It might be recommended in some women who are having difficulty becoming pregnant. A thin tube with a small balloon is inserted into the cervix, which can be inflated to keep the catheter in place. This process may sometimes make women feel faint or have period pain, so you should allow extra time to rest after the test.
We recommend you take the following medications approximately 30 minutes prior to your scheduled appointment: Buscopan 10mg tablets (take 2 tablets) and Nurofen 200mg (take 2 tablets)
The Buscopan tablets can help the uterus to relax and make it easier to insert the cannula into the cervix. They are generally well tolerated although they can give you a dry mouth.
Nurofen tablets are anti-inflammatory tablets that are also generally well tolerated but are not recommended if you have stomach ulcers. Both tablets are available over the counter at your local chemist.
It is important to perform this test at the correct time in your cycle to minimise the chance that the procedure itself may unintentionally interrupt a pregnancy. The procedure can be performed between day 2 and day 9 of the menstrual cycle in women who have a regular 28-day menstrual cycle.
In order to book the procedure at the correct time, it is important that you contact us on the first day of your period (or the Monday after your first day if your period starts on the weekend). We will then confirm an appointment date.
Tubal Patency assessment

We can perform ultrasounds on twin pregnancies at any of the stages of pregnancy including for:
- Early pregnancy
- First trimester Morphology scan
- Mid-trimester Morphology scan
- Third trimester scan
In addition to this, we pay special attention to the placentas and sacs of the twins to determine if they are sharing a placenta or whether there are two separate placentas. The type of twins a mother has will determine the frequency and degree of monitoring required for the pregnancy.
At Western Imaging for Women, our fetal medicine specialist obstetricians have particular expertise in managing twin pregnancies.
We recommend that otherwise uncomplicated twin pregnancies with separate placentas (dichorionic diamniotic twins) have ultrasound scans performed every 4 weeks after 20 weeks. Uncomplicated twin pregnancies with a shared placenta (monochorionic diamniotic twins) have ultrasound scans performed every 2 weeks from 16 weeks.
The frequency of ultrasounds may increase if complications are detected.
